3D Anatomic Modeling: Making surgery more precise, efficient and successful

Robert Spulak, Ph.D., worked for almost four decades as a physicist and manager at Sandia National Laboratories in Albuquerque, New Mexico. He has degrees in physics, astronomy and nuclear engineering. But farming is in his blood.
As a kid growing up in Iowa, Robert loved visiting his grandfather’s and uncle’s farms in Minnesota. As an adult, he raised sheep, put in an (ultimately unsuccessful) offer on 80 acres of Iowa farmland and started a Master of Agriculture correspondence program. So when an older cousin offered to pass on one of the farms Robert visited as a child, Robert, nearing retirement, was ready to finally dedicate his time to farming.
But Robert’s farming dreams came under threat in 2018, when an annoying pain throughout his left leg turned out to be a rare form of bone cancer known as chondrosarcoma in his pelvis. The cancer had not spread, and treatment required surgical resection of the bone. Standard of care would be to remove the entire hip joint, including part of the pelvis and femur, without reconstructing it. After this type of surgery, scar tissue forms in the space and supports weight, creating what’s known as a flail hip. But mobility and function are limited — making many of Robert’s planned farming tasks implausible.
When researching alternatives, Robert found that Mayo Clinic had been developing metallic pelvic implants to reconstruct the pelvis and hip after removing large amounts of bone.
“Since I was from the Midwest, I already knew of Mayo’s stellar reputation,” says Robert. “And since Mayo was located in Minnesota, I expected some sympathy for my desire to have enough functionality to farm.”
In September 2018, Peter Rose, M.D. (OR ’06), chair of the Division of Orthopedic Oncology at Mayo Clinic in Minnesota, and his surgical colleagues Matthew Abdel, M.D. (OR ’12), the Andrew A. and Mary S. Sugg Professor of Orthopedic Research, and Karim Bakri, M.B.B.S. (S ’10, PLS ’12), performed the 14-hour surgery and successfully resected the cancer and reconstructed Robert’s hip, pelvis and muscular envelope — preserving Robert’s farming dreams.
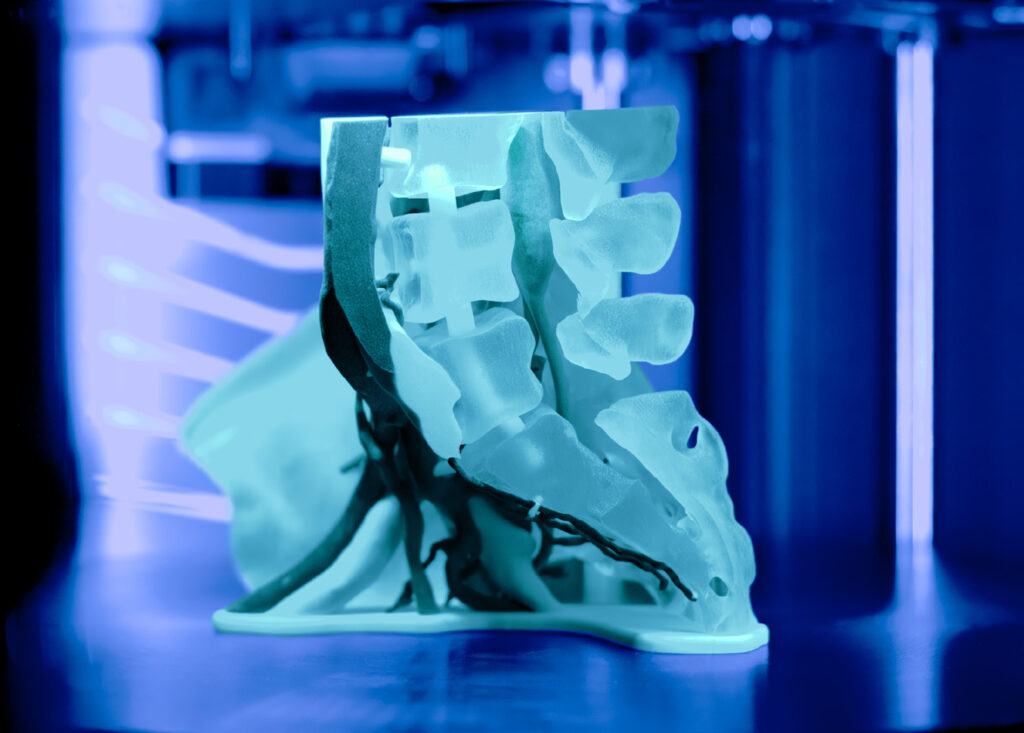
Dr. Rose is an experienced surgeon, but he had extra help: Mayo Clinic’s Anatomic Modeling Unit (AMU) in the Department of Radiology provided a 3D model of Robert’s hip anatomy and tumor, created a custom surgical cutting guide to provide an exact resection and worked with an orthopedic implant company to design a custom pelvic implant. Robert’s case is just one example of the AMU’s huge impact across surgical practice at Mayo Clinic.
Every year, the AMU in Minnesota produces about 1,000 anatomic models and 1,200 cutting guides, often on a tight timeline to accommodate urgent surgeries. These products can help make nearly every type of surgery — especially uncommon or complex surgeries — more precise, efficient and successful.
“A picture is worth a thousand words, and a model is worth a thousand pictures. This technology, it’s really all about the patient,” says Jonathan Morris, M.D. (RD ’06, RNEU ’07), co-founder and medical director of the AMU in Minnesota. “3D printing has changed what we can do for them and how we do it.”

“ A picture is worth a thousand words, and a model is worth a thousand pictures.”
– Jonathan Morris, M.D.
THE 3D CATALYST
3D printing at Mayo Clinic goes back to 2006, when surgeons and radiologists were preparing for a surgery to separate twin infants conjoined at the chest and abdomen. Surgeons from different subspecialties had to collaboratively plan the operation — a difficult prospect over 2D images, especially for organs such as a shared liver.
“One of the surgeons said, ‘Can we make a physical copy of their liver?’ And they said, ‘Well, why don’t we 3D print it?’” says Dr. Morris.
The team tried outsourcing the 3D printing, but the result was disappointing: it didn’t even look like a liver. Instead, Mayo’s Department of Engineering worked with radiologist Jane Matsumoto, M.D. (MED ’80), and other physicians to create a 3D model of the twins’ fused liver, giving the team a close look at the vascular and biliary anatomy of the organ. The twins were ultimately separated successfully.
“It was the first time that a group of surgeons could hold a patient’s liver in their hands outside the body,” Dr. Morris says. “That 3D-printed liver was the catalyst of what we’ve become today.”
It spurred the creation of the AMU in Minnesota and, eventually, at Mayo Clinic’s campuses in Arizona and Florida. The AMUs rely on collaborations between physicians, researchers, engineers and technologists, and they bring top-tier 3D printing facilities to the hospital, a model known as point-of-care manufacturing.
Getting here required tremendous effort. The Minnesota AMU team had to create custom infrastructure for the manufacturing spaces with careful airflow design and anterooms so that powder, polymers and glues wouldn’t contaminate the patient areas. The team set up batch contracts for raw materials and off-premise validation testing for biocompatibility, sterilization and cytotoxicity. They hired engineers, healthcare technology maintenance staff and radiology technologists and set up quality control protocols for their 3D printers. Today, Minnesota’s AMU contains about 8,000 square feet of manufacturing space — with 18 staff, 15 industrial 3D printers, and a room full of post-processing equipment such as lye baths and vapor smoothing. The Arizona and Florida units each include about 1,000 square feet.
“We have one policy: The door is open,” says Dr. Morris. “Any surgeon or clinician at Mayo Clinic can come in and ask a question about a unique patient problem. And we bring technology to bear on the needs of the patient.”

NO MENTAL GYMNASTICS
3D anatomic models help surgeons explain, plan or even practice surgery. Holding an anatomic model before beginning surgery may help a surgeon understand anatomic anomalies and even change the surgical approach. A systematic review found that over 80% of studies examining the use of 3D anatomic models in surgical planning noted better clinical outcomes when the models were used.
“It’s much easier to give them this than to say, ‘Why don’t you take these 13,000 images from a CT scan, marry them to 1,500 images on an MRI scan, maybe another 2,000 images on a PET scan and make a complex 3D object in your mind?’” says Dr. Morris. “We just hand them the model and, by mixing haptic perception with visual perception, a new understanding develops. There’s no mental gymnastics.”
In addition, the AMU creates digital “twins” of the patient’s anatomy, allowing virtual surgical planning on a computer. Thus, very precise cuts in the bone or soft tissue can be planned outside the operating room before the procedure.
Digital surgical plans can then be transformed into custom, patient-specific designs for cutting guides to precisely resect tumors or cut out exact segments of bone. These are then manufactured with biocompatible, sterilizable materials on one of the AMU’s 3D printers.
The digital surgical plans can also be used to create custom titanium implants in partnership with external companies with titanium 3D printing capabilities. Other times, 3D anatomic models created by the AMU are used to pre-bend implants, which can save time in the operating room.
The AMU has conducted studies showing that these services drive surgical confidence and result in less time under anesthesia, less time in the OR and less blood loss. These techniques can also lead to greater organ preservation when resecting tumors involving the kidneys, lungs or liver. In orthopedic oncology surgeries, AMU’s services can lead to better bone preservation — sometimes allowing surgeons to spare a limb otherwise slated for amputation.
“We provide a tool that allows the surgeon to understand things in a way that’s easy for them — and then allows them to do what they do even better than they already do it,” Dr. Morris says.

The 3D model of Robert Spulak’s pelvic chondrosarcoma (in green) helped Robert’s surgeon Peter Rose, M.D., visualize and plan the surgery to remove the cancer while protecting major blood vessels (in red and blue) and nerves (in yellow). The model was created by the Anatomic Modeling Unit (AMU) in the Department of Radiology at Mayo Clinic in Minnesota.

The patient-specific cutting guide (in orange) created by the AMU for Robert’s surgery was carefully designed to fit the contour of his bone and preserve the femoral and sciatic nerves and as much of the native bone above the tumor as possible.

The AMU and Dr. Rose worked with an orthopedic implant company to design a custom pelvic implant (in silver) that exactly matched the planned cut and guided the fixation screws into the remaining bone. The custom implant reconstructed the pelvis and hip, allowing weight bearing after large amounts of bone had to be removed to resect the chondrosarcoma.
Learn more about how 3D anatomic modeling works
First, a surgeon decides the clinical case warrants a 3D anatomic model, cutting guide or custom implant. The surgeon orders this from the AMU in the electronic medical record just like any other test at Mayo Clinic.
The patient is then triaged to one of several CT and MRI scanners where radiology protocols have been developed for this purpose, as the protocols are slightly different than those used for diagnostic scanning. The scans are then digitally transferred to the AMU, and specially-trained CT and MRI technologists (segmenters) take the images and convert them into a patient-specific virtual 3D model or “digital twin” of the anatomy and pathology. A single scan may have 13,000 images; technologists — or increasingly, custom Mayo-developed artificial intelligence algorithms — go through each image, segmenting each anatomic and pathologic feature of interest into unique 3D files. These are used to create full-color 3D digital models with each anatomy assigned a different color. For example, coloring the pelvic bone as tan, tumor tissue as green, nerves as yellow, and blood vessels as red and blue. Then one or more printer technologies are used to print a life-size 3D model of the patient’s anatomy layer by layer, a process known as additive manufacturing. Using subtractive manufacturing to create a 3D model would be akin to chiseling away stone to reveal a statue.
The various 3D printers in the AMU use different technologies, including lasers hardening liquid resins, UV light curing photopolymers, lasers melting nylon powders and electron beam melting. Each type of printer has its own strengths and is chosen depending on the job at hand — such as whether it’s a model for surgery planning, training or patient education.
The patient is then triaged to one of several CT and MRI scanners where radiology protocols have been developed for this purpose, as the protocols are slightly different than those used for diagnostic scanning. The scans are then digitally transferred to the AMU, and specially-trained CT and MRI technologists (segmenters) take the images and convert them into a patient-specific virtual 3D model or “digital twin” of the anatomy and pathology. A single scan may have 13,000 images; technologists — or increasingly, custom Mayo-developed artificial intelligence algorithms — go through each image, segmenting each anatomic and pathologic feature of interest into unique 3D files. These are used to create full-color 3D digital models with each anatomy assigned a different color. For example, coloring the pelvic bone as tan, tumor tissue as green, nerves as yellow, and blood vessels as red and blue. Then one or more printer technologies are used to print a life-size 3D model of the patient’s anatomy layer by layer, a process known as additive manufacturing. Using subtractive manufacturing to create a 3D model would be akin to chiseling away stone to reveal a statue.
The various 3D printers in the AMU use different technologies, including lasers hardening liquid resins, UV light curing photopolymers, lasers melting nylon powders and electron beam melting. Each type of printer has its own strengths and is chosen depending on the job at hand — such as whether it’s a model for surgery planning, training or patient education.
A TRUSTWORTHY TUMOR GUIDE
In orthopedic oncology surgery, Dr. Rose says, the name of the game is resecting a bone tumor in one piece with a proper margin.
That’s easier in some surgeries than others. For a tumor in a long, straight bone like the tibia, Dr. Rose can use an X-ray camera, find the ankle or knee joint, and use that as the starting point to measure the appropriate number of centimeters to the tumor.
“When you start to get into something like the pelvic bone, which is a bone that curves in multiple planes at once, there are no defined landmarks that we can access well in surgery,” he says. “And there’s a host of other structures to consider: your bowel, your bladder, your pelvic organs, muscles, nerves, blood vessels — those all make it more difficult.”
Years ago, the best Dr. Rose could do to visually collaborate with other surgeons for this type of procedure was examine the imaging, pull out his pelvis model coated in whiteboard material, take a dry erase marker and sketch out the planned resection.
“Quite frankly, we were successful as far as our ability to get the cancers out reliably, but we were probably taking in some cases more than was necessary, as we had to be safe,” says Dr. Rose.
But life-size, 3D-printed, patient-specific models provide a “better intuitive understanding of cancers: where they are and what we can and can’t save,” Dr. Rose says. In Robert’s case, the AMU was not only able to make a 3D model and digital plan to assist with Dr. Rose’s surgical planning, but a cutting guide that was carefully designed to fit the contour of his bone and preserve the femoral and sciatic nerves and as much of the native bone above the tumor as possible. The AMU and Dr. Rose also worked with an orthopedic implant company to design a custom-made pelvic implant that exactly matched the planned cut.
Dr. Rose was not the only one considering the 3D model of Robert’s pelvis before surgery; Robert himself got to examine the model, cutting guide and custom implant. Seeing that “they could use the models to precisely cut and precisely place the implant,” gave Robert “a lot of confidence,” he says.
Dr. Rose says these models are invaluable in explaining pathology and upcoming procedures to patients.
“Many of the patients who are referred to us have very rare tumors, and they may not have a good understanding of their extent and relationship to surrounding critical structures,” Dr. Rose says. “The ability to sit down with them with a model that shows their exact anatomy can be very valuable to build trust and comfort.”
Looking forward, Dr. Rose says that he and his colleague Matthew Houdek, M.D. (OR ’16), Division of Orthopedic Oncology at Mayo Clinic in Minnesota, will continue to innovate and bring musculoskeletal tumor patients the best hope of cure and restoration of function.
FARMING DREAMS FULFILLED
Robert’s recovery was long and, at times, arduous. But his dream of farming motivated him through five weeks in the hospital, seven weeks of frequent outpatient therapy, months of continuing physical therapy at home, and years of exercise to build up his leg and core strength. His current function is incredible: he walks with a near-normal gait and without a cane, though a bit slower than before. He’s in his third year of farming corn and soybeans. He can carry a sack of seed corn, climb up into his tractor, repair large machinery and — with the help of a special back brace — pick up big rocks to clear his fields. While he’s still “on the steep part of the farming learning curve,” he’s enjoying himself.
“There are a lot of problems you have to solve, including mechanical breakdowns and what varieties of seed to plant,” he says. “I like figuring out how to overcome these obstacles.”

Want to take a closer look?
In addition to physical models and digital surgical plans, Mayo Clinic’s Anatomic Modeling Unit can create interactive models accessible by QR code. Use your phone to scan the QR codes and take a closer look at the models created for Robert.
READ THE ENTIRE BENCH TO BESIDE SERIES
This story appears in the latest issue of Mayo Clinic Alumni magazine. You can read or download a PDF of the issue here.
Mayo Clinic alumni are entitled to the print version of the quarterly magazine. If you’re not receiving the magazine, register or log in to your online MCAA profile to make sure your address is correctly entered. Or contact the Alumni Association at mayoalumni@mayo.edu or 507-284-2317 for help.
Credit: Photos of Robert Spulak by Ackerman + Gruber